How the Opioid Crisis Has Hit Headwaters
It’s not just a big city problem. Here’s how local communities are trying to stem the flow of pain pills.
Susan Smith never intended to become hooked again. In her late teens and early 20s, she had battled substance abuse, then stayed clean for 20 years while living in the Headwaters region.
But when Smith was 50, she was prescribed a benzodiazepine for anxiety. The “downer” nudged her addictive tendencies back to the surface, and before long she was adding Valium, marijuana, alcohol and oxycodone to the mix – creating a potentially lethal drug cocktail.
It was the oxycodone, which belongs to a potent class of drugs called opioids and is similar in chemical makeup to morphine and heroin, that Smith (she declined to use her real name to protect her privacy and that of her family) found was hardest to beat. When she tried to stop on her own, she became so ill she couldn’t work and cycled right back into using.
“I got really scared, so I reached out for help,” Smith says. She found that help through Orangeville’s Family Transition Place and has been clean now, except for a low, legal prescription of the original anxiety medication, for about six months.
Looking back on the past few years, Smith says she feels lucky she didn’t encounter fentanyl, oxycodone’s more concentrated and far more deadly sibling.
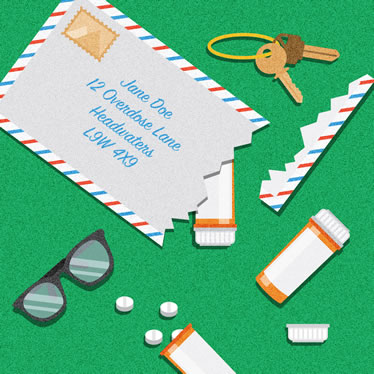
When OxyContin was remade in a crush resistant formula, many pivoted to illicit opioids created in illegal labs and mailed in small packages, even greeting cards. Illustration by Ruth Ann Pearce.
Now a growing focus of illicit drug use in Ontario, fentanyl is a painkiller prescribed by doctors, usually in the form of pills or therapeutic patches. Stolen or unused prescriptions are available on the black market, along with versions of fentanyl created in illegal laboratories. The drug can be a hundred times more potent than morphine, one of the original opioids. Traces of fentanyl have been found cut into street drugs, including heroin, cocaine, crystal methamphetamine and ecstasy, as well as into counterfeit Percocet, OxyContin and Dilaudid pills. Health professionals across the country are sounding the alarm that these drugs, tiny amounts of which create pleasing sensations of euphoria, have led to a growing wave of overdoses and deaths.
Fentanyl has now arrived in Headwaters, and if it worms its way deeper, there will be more Susan Smiths in our midst, though fewer may live to tell the tale.
Mapping an opioid epidemic
The growing opioid crisis is a vexing, multiheaded beast. First responders, public health officials and educators are working to teach the public about the dangers of opioids and how to mitigate the risks. Governments are earmarking new funds for more harm reduction and addiction treatment services to help those most likely to overdose. In late August, for example, the Ontario government pledged to spend an additional $222 million over three years for these and other programs related to opioid use.
What are opioids?
Opioids is a broad term describing all drugs based on naturally occurring compounds found in opium poppies. Opiates are drugs, such as codeine and morphine, created by separating and purifying various chemicals in the poppy. Opioids include all opiates, along with synthetic drugs designed to work like opiates, such as fentanyl, heroin and oxycodone.
Opioids work by attaching to brain receptors that modify our reaction to pain, says Dr. Kate Bingham, associate medical officer of health for Peel Region.
Until about 15 years ago, opioids were mostly prescribed to cancer and palliative-care patients. Canada now has one of the highest opioid prescription rates in the world, with opioids being used to treat everything from the sensation of breathlessness for patients with chronic obstructive pulmonary disorder (COPD) and pulmonary fibrosis to pain after dental surgery, lower back pain and other forms of chronic pain, which affects about 15 to 19 per cent of Canadians.
— TP
In addition, the medical community has been working to dial back the number of legal opioids being prescribed, both to stem the flow of unused meds into the street drug network and to protect patients who may be harmed by long-term use of high doses.
To help achieve this goal, Health Canada and the Canadian Institutes of Health Research jointly funded a project by the Michael G. DeGroote National Pain Centre at McMaster University in Hamilton. Its purpose was to develop new guidelines for prescribing opioids. The researchers who formulated the guidelines, which were published in the Canadian Medical Association Journal in early May, noted that dispensing of prescription opioids for pain relief nearly tripled across Canada between 2001 and 2014. From 2001 to 2003, opioid prescriptions averaged 10,209 daily doses for every million people. From 2012 to 2014, this number rose to an average of 30,540 daily doses for every million people.
A new online tool created by Public Health Ontario graphs the number of emergency-room visits, hospitalizations and deaths attributed to opioids in each provincial public health jurisdiction. In the two jurisdictions that serve Headwaters – Wellington-Dufferin-Guelph Public Health and Peel Public Health – the lines on the graphs are trending relentlessly upward.
In Peel, the first 23 recorded deaths due to opioid overdoses took place in 2005, at a rate of 1.9 deaths per 100,000 people. By 2015, the number of deaths had risen to 53, a rate of 3.8 deaths per 100,000. Numbers recorded by Wellington-Dufferin-Guelph Public Health follow a similar pattern, with four deaths in 2005 doubling to eight in 2015. (Though it is impossible to determine the source of a given opioid responsible for an overdose, most overdoses happen to people suffering from addiction and using drugs not prescribed by a doctor.)

The top priority is ensuring first responders and people at risk have access to naloxone, the injectable drug that can resuscitate overdose patients in one or two minutes. Illustration by Ruth Ann Pearce.
Tom Reid, chief of Dufferin County Paramedic Service, says that in 2016 he and his team responded to a total of 64 overdose calls involving drugs or alcohol or both. They administered the opioid antidote naloxone (brand name Narcan) six times. As of mid-August this year, they had already answered 45 overdose calls and given naloxone nine times. Two opioid-related deaths have been confirmed by a coroner.
These statistics belie the prejudices many of us hold toward drug abusers. Accidental overdoses affect people of every age and from every walk of life. Most of those affected are between the ages of 20 and 40.
“We have had kids, there’s no question, some really tragic cases,” says Reid. “But it’s not just a teenager problem. It’s a community problem.”
How opioid addiction happens
Why do opioids appear to be having such devastating consequences after being prescribed for fairly universal health complaints? And why are street versions of the drugs proving more deadly to addicts than other illicit substances?
Within a couple of days of taking opioids, a person becomes physically dependent on them, says Dr. David Juurlink, head of clinical pharmacology and toxicology at Sunnybrook Health Sciences Centre. As with alcohol, patients and users also become more tolerant of opioids, requiring higher and higher doses to achieve the same effects.
“When they stop taking them, they get sick,” says Juurlink, who served on the steering committee that helped develop the new opioid prescribing guidelines. “In some people that sickness manifests as abdominal pain or pain at the site of an old injury.”
“If you were my patient and I had you on oxycodone for a month and we decided to stop it, you would feel miserable for weeks, not days,” he says. “You’d have abdominal pain and diarrhoea and you would have trouble sleeping. In some instances people describe feeling suicidal. It’s incredibly dysphoric. Take the worst flu you’ve had and multiply it by 10 or 20.”
But all these symptoms can be made to go away by simply taking another pill, he says.
It didn’t have to be this way. There is plenty of blame to go around, starting with the pharmaceutical companies that claimed opioids were safe and persuaded many doctors to start prescribing them widely.
Dr. Kate Bingham, Peel Region’s associate medical officer of health, recalls the advice handed out when she was at medical school: “The story at that point was that we had been undertreating pain for a long time and physicians weren’t compassionate about people’s pain or adequately caring for people.”
Over the past 20 years, jurisdictions across North America have been successfully suing Purdue Pharma, makers of OxyContin, the opioid widely blamed for kicking off the epidemic of abuse. This past spring, the company agreed to settle a class-action suit launched on behalf of about 1,500 Canadians who became dependent on the drug when the risks weren’t disclosed to them. But the $20 million settlement, which included $2 million earmarked for provincial health plans, is a fraction of the medical costs associated with getting patients off the drug. By comparison, pharmaceutical companies in the United States have paid upwards of $35 billion to federal and state governments over the past 25 years.
“The idea that we could take the opium poppy, tweak it chemically and give it to people for months or years at a time at extremely high doses, without any studies to back us up, was really based on wishful thinking,” says Juurlink.
In 2012, when OxyContin was taken off the market in Canada and remade in a crush-resistant formula that didn’t lend itself to abuse, many people addicted to the drug pivoted to other, more dangerous options, especially illicit opioids created in illegal labs across North America and China, and mailed in small packages, even in greeting cards.
First priority: Help the addicted
At least 2,500 Canadians died of opioid overdoses in 2016, according to the Public Health Agency of Canada. And this number is likely to grow to 3,000 this year, says Juurlink. “We’ve lost around 30,000 people in Canada in the last 20 years.”
Kristy Fearon, a social worker and addiction outreach counsellor at Family Transition Place, says that when she takes clients’ substance use histories, 90 per cent say their opioid addiction started when they were given a prescription after surgery, a car accident or a dental procedure. Opioids, says Fearon, were handed out “like Tic Tacs.”
And people who start taking them recreationally eventually find themselves taking them to avoid withdrawal symptoms, even if they’re no longer getting a particularly good high from the drug, says Bingham.
Though Fearon started her work four years ago as part of a Family Transition Place program to help pregnant and parenting women with opioid addictions, the program now serves a broader range of women. Many of her clients come to addiction via the mental pain of abuse and trauma.
A mother’s fear of losing her kids to the Children’s Aid Society can further drive women users underground. Another major challenge for women in Headwaters, says Fearon, is their vulnerability to the local online sex trade. Though this problem is mostly invisible, some of the women Fearon sees face enormous hurdles in trying to reclaim their lives. As much as they may want to leave the fast-cash trade, she says, “I get texts saying, ‘I can’t [kick my addiction]. It’s easier to go back to the trade.’ I tell them, ‘I’m still here if you need me.’”
Hearing this, it’s easy to see why Fearon and others on the front lines advocate a harm-reduction approach, which includes safe spaces and clean equipment for using drugs. But the top priority is ensuring first responders and people at risk of overdosing and dying have access to naloxone – the injectable drug can resuscitate an overdose patient in one or two minutes.
Tom Reid explains it isn’t the toxicity of a drug like fentanyl that kills or causes brain damage during an overdose. “People don’t die from the drugs. They die from forgetting to breathe,” he says, adding that his teams always carry naloxone.
Ontario’s Ministry of Health and Long-Term Care has made naloxone available over the counter at all pharmacies in Ontario, and in March the Peel Works Needle Exchange Program started distributing the nasal spray form from its mobile van.
Reid adds that naloxone’s effects aren’t long lasting. Even after patients are revived, getting them to a hospital emergency department is crucial.
To assist others like Smith before they get to that harrowing stage, Family Transition Place helps clients find services such as medical detox programs (though the wait can be as long as six months), talk therapy such as cognitive behavioural therapy and psychiatric treatment, or drug therapies such as methadone and Suboxone, both of which can help ease people off opioids while reducing the shock to the system. Users do not have to be clean and sober when starting a program, and complete abstinence is not necessarily the goal. Helping a client cut down or use only on weekends may be the place to start.
Fearon, whose current caseload sits at 45, asks newcomers – some walk in, others are referred by other agencies or as part of a parole arrangement – to set their own goals and work at a reasonable pace. She frequently uses a common therapy tool called the “miracle question.” She says, “I ask, ‘If you woke up tomorrow and everything was as perfect as you wanted it, what would it look like?’ From there, I ask ‘What is it we need to be doing [to help get you there]?’”
Country conundrum

Known for its use in remote Indigenous communities, telemedicine is in demand anywhere without readily available walk-in clinics. Illustration by Ruth Ann Pearce.
Ideally, people struggling with addictions would have access to the same kinds of walk-in services available in large urban centres. Country dwellers seeking help for addictions may have had their driver’s licence suspended for impaired driving or be unable to afford transportation. For them, a psychiatric appointment in Brampton might as well be a continent away.
To tackle these barriers, Fearon often takes her “office” mobile. She will take a client to doctors’ appointments or speak to a client’s husband or family to explain treatment. Over Wi-Fi on the laptop in her office or at a client’s home, she also sets up remote medical and psychiatric appointments using the Ontario Telemedicine Network. Known for its use in remote Indigenous communities, telemedicine is in demand anywhere without readily available walk-in clinics. “It’s really taking off,” says Fearon. “Younger doctors who are tech savvy are wanting to do it. There is a lot of shifting that is happening, thankfully. But we have a long way to go.”
Other approaches rely on a telephone that never goes unanswered. Smith says one of the most effective strategies she learned at Family Transition Place was how to ride out a period of intense craving. She’d call the agency at 4 a.m. just to chat or even just to breathe slowly on the phone with a staff member at the other end of the line. Fearon compares this technique to trying to delay eating a food you’re determined to avoid. Says Smith, “I want families to know there is help, and it’s hard because it’s a mean, hard drug, but through great services … we can respond and give people hope.”
About that pain
At the same time as the illegal use of opioids is rising, scores of legal opioid users who are taking their pain pills as prescribed, under a doctor’s supervision, may wonder anxiously about the future of a treatment increasingly characterized as risky and unsafe. Side effects now being more widely discussed include falls, car accidents, fractures, low testosterone levels and depression.
The new Health Canada guidelines focus on the use of opioids for non-cancer care patients and encourage physicians to prescribe opioids as a last resort. Maximum doses equal to 90 mg of morphine are suggested, rather than the current 200 mg. The guidelines also suggest tapering to lower doses or moving patients to other opioids for shorter periods.
Those who must remain on high doses or who drink alcohol or take sleeping pills or other sedatives, Juurlink advises, should keep a naloxone kit at home, just in case. The Health Canada guidelines suggest doctors discuss this option with patients – but the guidelines also point out there is scant evidence this strategy saves lives. Nevertheless, in late August, the American Medical Association’s opioid task force updated its guidelines to recommend co-prescribing naloxone, a position that aligns with the advice of the World Health Organization and other health agencies.
Whether measures like these will help change the course of the current crisis is unclear. Juurlink says he has encountered patients on doses of 5,000 mg. “You think, ‘Wow, this person is going to be on opioids for the rest of their life and they might indeed die from their therapy one way or another. If their car goes off the road, or they fall asleep and don’t wake up, no one’s going to blame opioids for that.’”
Reducing demand
Back here in Headwaters, community organizations are boosting their efforts to give young people and their parents as much information as possible about the risks of opioids. According to the most recent figures collected by the Centre for Addiction and Mental Health as part of the organization’s continuing survey of drug use among Ontario youth, nearly 68 per cent of Grade 7 to 12 students surveyed had tried alcohol at some point. About 24 per cent had tried marijuana and 12 per cent had used prescription opioids non-medically.
On a warm evening in June, about two dozen parents gathered in an auditorium in Orangeville’s Westside Secondary School for a presentation by local police, paramedics and drug counsellors. Presented to students across Dufferin during school hours, the information was repeated for families in the evenings.
One powerful slide looming on the projection screen showed how a deadly dose of fentanyl looks like a few grains of salt, whereas a deadly dose of an even more concentrated opioid called carfentanil, developed as a veterinary anesthetic for elephants and other enormous animals, can be as small as a single grain.
But the most harrowing part of the night was when Orangeville mother Brigitte Pelkey spoke about losing her 24-year-old son to an opioid overdose last fall. “He was a normal teenager,” she says, her voice breaking. “Then he started withdrawing.”
She said her son became addicted when opioids were prescribed after dental surgery and, later, after a car accident. He then sought out fentanyl patches. He would overdose and be discharged from hospital with no plan for how to help him and no guidance from doctors, not even a pamphlet.
“I got nothing,” she said through tears.
Constable Scott Davis, community services and media relations officer for the Orangeville Police Service, was one of the event’s organizers and has gotten to know Pelkey. “I’m a dad,” Davis said in a later conversation. “I think of my own kids and how it could be anybody’s kid. I didn’t know Brigitte’s son, but from what I’ve learned, he was a good kid.”
Some wary parents at the talk openly suggested that police intercept kids’ mail to look for drugs or that school officials search lockers to root out drugs. Instead, says Davis, “Education is the best way this issue’s going to be resolved or at least reduced.”
And after 22 years on the job, he urges parents to examine their own behaviour. If you drink alcohol or use any drug recreationally, consider your actions and the messages you’re sending, especially to underage kids.
For the parents who gathered to chat after the presentation, Pelkey’s words expressed their worst fear: losing a child. One mother said she keeps her Grade 9 son home from house and bush parties, but she knows she’ll soon need more tools to help him stay safe. Still, the conversation did feel like the start of something. The community responds when things become personal, when a death involves a neighbour and is more than a statistic in a far-off city.
On August 31, the experts who pulled together the presentation capped the summer by staging the first International Overdose Awareness Day in Orangeville. The event was inspired by an Australian nonprofit initiative that focuses on raising awareness and paying tribute to victims in a permanent online memorial.
“When you see the pain of a family after we lose someone in such a preventable way, I feel for them,” says Tom Reid. “They all have family who love them. It seems so preventable and so tragic. Anything we can do to promote good choices and education around this is something we should all do as a community.”
Learn more: Mental health issues in Dufferin
More Info
You are at risk of an opioid overdose if
- you’re taking prescription opioids that were not prescribed for you and could be too strong for you
- you’re buying opioids on the street and you don’t know how strong they are
- you’ve bought street drugs laced with opioids
- you’ve overdosed on opioids in the past
- you’re mixing opioids with other downers such as alcohol and benzodiazepines, or “benzos” (Valium, Xanax, etc.)
- you’ve stopped using opioids for a while, which has lowered your tolerance
- you’ve just been released from jail and haven’t used opioids in a while
- you’re using opioids by yourself.
— Government of Ontario
How to prevent an opioid overdose
- Keep prescriptions away from children, young people, and other adults in your home.
- Don’t give anyone your prescription opioids or take opioids prescribed for someone else.
- Don’t mix drugs or take drugs with alcohol.
- Don’t use opioids when by yourself.
- If you switch to a stronger opioid, use less and do a test dose.
- If you’re using opioids after cutting down or not using for a while, start low and go slow.
— Government of Ontario
Where to find help and resources
Related Stories

The Yin and Yang of Well-Being
Mar 23, 2015 | | LeisureAs alternative therapies move into the mainstream and options expand, it’s harder than ever to know what choices make sense for your health. Nicola Ross went on a personal journey to find out.

Shadowland: Mental Illness in Dufferin County
Jun 18, 2009 | | Back IssuesMental illness is a lonely, often hidden disease – all the more so in Dufferin County where services are fractured and funding is, abysmally, the lowest in the province.








I had the pleasure of reading the article “How the Opioid Crisis Has Hit Headwaters.”
We appreciate light being cast on the issue of addiction but were dismayed that our pharmacy was not consulted for this article. We work closely with the Family Transition Place and actually have many mutual patients.
Pharmacists are the most accessible health care providers. We have over 20 years of experience in the addiction field and with us being the only clinic in town to serve the very same issue this article thankfully highlighted, we feel we could add to the overall positive message.
Here’s what we’re doing to help:
Medication disposal
– We offer free medication disposal services to the community for unused and expired medications. This is important so that these medications don’t end up in the wrong hands, enter our water supply and pollute the environment.
-We also can visit an individual at home to do a full “medication reconciliation,” whereby unused/expired medications are removed in a safe manner.
Education
– We educate patients about the safe use of all medications and offer (either in home or at the pharmacy) in-depth medication review appointments for individuals with a valid health card.
– We provide information on how medication(s) can effect someone who is not intended to take it (especially true for highly addictive medications like opiates).
– We’re accessible. Our website (broadwaypharmasave.com) provides information, as does our Facebook page and Twitter account @orangevillerx. Some patients even choose to directly engage with the pharmacist by using a platform such as Facebook Messenger.
Addiction help
– We offer information to patients seeking help with dependence or addiction.
– We shelter individuals from the stigma of addiction by providing an inclusive, respectful environment.
– We work closely with the Freedom Trail Addiction Clinic in Orangeville as well as two other clinics in other jurisdictions (Horizons Clinic in Georgetown and New Direction Clinic in Brampton). We also work closely with the Centre For Addiction and Mental Health which has many tools and counselling points to inform patients in an approach that is non-judgemental and inviting.
Harm reduction
– We use tools such as the Narcotic Monitoring System (NMS) to stay on top of irregularities, poly-pharmacy or poly-prescribing.
– We stay in touch with prescribing doctors and discuss any irregularities, or prescription-seeking behaviour and invite discussion with the patient about high-risk behaviour.
– We offer methadone and suboxone treatment for opioid dependence.
– We distribute naloxone for free to anyone with a valid health card and educate anyone at risk or who works/lives with people at risk.
– We share what to look for in a potential opiate overdose (signs and symptoms), how and where to inject the naloxone, how much time naloxone can take to work, what to look for after administering the injection, what drugs naloxone can work for and what drugs it can’t work for.
I hope this feedback provides a clear picture of what we offer locally in Orangeville. Of course, we are always of the mindset that learning is a lifelong journey so are open to suggestions to improve and also address anything we can that doesn’t seem clear.
Manveer (Manny) Dhillon, Pharmacist from Broadway Pharmacy, Orangeville on Oct 13, 2017 at 12:30 pm |